IVF is a method of assisted reproduction in which a man's sperm and a woman's eggs are combined outside of the body in a laboratory dish. One or more fertilized eggs (embryos) may be transferred into the woman's uterus, where they may implant in the uterine lining and develop. Excess embryos may be cryopreserved (frozen) for future use. Today, IVF is used to treat many causes of infertility, such as endometriosis and male factor, or when a couple's infertility is unexplained. The basic steps in an IVF treatment cycle are ovarian stimulation, egg retrieval, fertilization, embryo culture, and embryo transfer.
During ovarian stimulation, "fertility drugs," are used to stimulate multiple eggs to grow in the ovaries rather than the single egg that normally develops each month Multiple eggs are stimulated because some eggs will not fertilize or develop normally after fertilization. Oral medications are less potent than injectable medications and are not as commonly used in ART cycles.
Timing is crucial in an IVF cycle. The ovaries are evaluated during treatment with vaginal ultrasound examinations to monitor the development of ovarian follicles .Blood samples are drawn to measure the response to ovarian stimulation medications.Generally, 8 to 14 days of stimulation are required. When the follicles are ready, hCG or other medications are given. The hCG causes the final stage of egg maturation so the eggs are capable of being fertilized. The eggs are retrieved before ovulation occurs, usually 34 to 36 hours after the hCG injection is given.
Up to 20% of cycles may be cancelled prior to egg retrieval. IVF cycles may be cancelled due to an inadequate number of follicles developing. Cancellation rates due to low response to the ovulation drugs increase with a woman's age, especially after age 35. Occasionally, a cycle may be cancelled to reduce the risk of ovarian hyperstimulation syndrome (OHSS). Treatment with a GnRH agonist or antagonist reduces the possibility of premature LH surges from the pituitary gland, and thereby reduces the risk of premature ovulation. However, LH surges and ovulation occur prematurely in a small percentage of ART cycles despite the use of these drugs. When this occurs, since it is unknown when the LH surges began and eggs will mature, the cycle is usually cancelled.
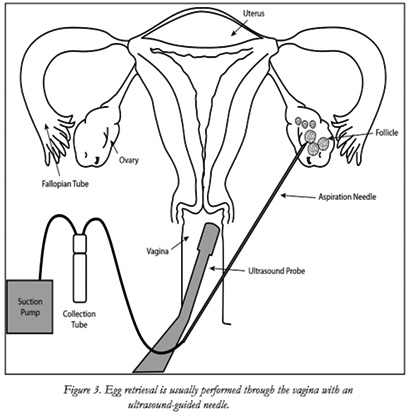
Egg retrieval is usually accomplished by transvaginal ultrasound aspiration, a minor surgical procedure that can be performed in the physician's office or an outpatient center. Some form of pain medication is generally administered. An ultrasound probe is inserted into the vagina to identify the follicles, and a needle is guided through the vagina and into the follicles.
The eggs are aspirated from the follicles through the needle connected to a suction device. Removal of multiple eggs can usually be completed in less than 30 minutes. Some women experience cramping on the day of the retrieval, but this sensation usually subsides by the next day. Feelings of fullness and/or pressure may last for several weeks following the procedure because the ovaries remain enlarged. In some circumstances, one or both ovaries may not be accessible by transvaginal ultrasound.
Sperm is separated from semen usually obtained by masturbation or in a special condom used during intercourse. Alternatively, sperm may be obtained from the testicle, epididymis, or vas deferens from men whose semen is void of sperm either due to an obstruction or lack of production.
Fertilization may be accomplished by insemination, where motile sperm are placed together with the oocytes and incubated overnight or by intracytoplasmic sperm injection (ICSI), where a single sperm is directly injected into each mature egg. ICSI Treatment is usually performed when there is a likelihood of reduced fertilization (e.g., poor semen quality, history of failed fertilization in a prior IVF cycle). Overall, pregnancy and delivery rates with ICSI are similar to the rates seen with traditional IVF.
Visualization of two pronuclei the following day confirms fertilization of the egg. One pronucleus is derived from the egg and one from the sperm. Usually 65% to 75% of mature eggs will fertilize after insemination or ICSI. Lower rates may occur if the sperm and/or egg quality are poor. Occasionally, fertilization does not occur at all, even if ICSI was used. Two days after the egg retrieval, the fertilized egg has divided to become a 2- to 4-cell embryo
By the third day, a normally developing embryo will contain approximately 6 to 10 cells. By the fifth day, a fluid cavity forms in the embryo, and the placenta and fetal tissues begin to separate. An embryo at this stage is called a blastocyst. Embryos may be transferred to the uterus at any time between one and six days after the egg retrieval. If successful development continues in the uterus, the embryo hatches from the surrounding zona pellucida and implants into the lining of the uterus approximately 6 to 10 days after the egg retrieval.
The next step in the IVF process is the embryo transfer. No anesthesia is necessary, although some women may wish to have a mild sedative. The physician identifies the cervix using a vaginal speculum. One or more embryos suspended in a drop of culture medium are drawn into a transfer catheter (a long, thin sterile tube) with a syringe on one end. The physician gently guides the tip of the transfer catheter through the cervix and places the fluid containing the embryos into the uterine cavity . The procedure is usually painless, although some women experience mild cramping.
After the eggs are retrieved, they are examined in the laboratory for maturity and quality. Mature eggs (Figure 4) are placed in an IVF culture medium and transferred to an incubator to await fertilization by the sperm.

IVF is the most effective treatment for women. During IVF, fertilization of eggs is done outside the body in our lab.
Couples are offered IVF for a variety of reasons, for example,because of damage to your fallopian tubes, endometriosis or poor sperm quality. It may even be that no specific cause can be found – when it is called ‘unexplained infertility’.
This is a very stressful time for couples and the couples have many questions about how to prepare for treatment and what to expect.
To help couples decide on what to do, we run pre-treatment sessions.
During these we talk you through the treatment steps so you can get an idea of what is involved and ask any questions before you make a decision. Please contact us to arrange a visit.
This is your treatment. We know you want to be fully aware of the facts and their implications so that you can make the right decisions.
Normally a woman produces one egg every month. This egg is released into the fallopian tube where it may be fertilised following sex. The fertilised egg then travels to the womb. If the resulting embryo implants, the woman will become pregnant.
During ivf, stimulation of the ovaries is done to produce multiple follicles. Each follicle contains one egg. The chances of pregnancy are increased if more than one egg can be obtained and fertilised.
The response to stimulation is monitored by ultrasound scan measuring the number and size of the developing follicles in the ovaries and by measuring the blood oestrogen level.
The ultrasound does not show the eggs themselves, but the fluid-filled sacs (follicles) containing the eggs. The ultrasound scans are performed at intervals during the treatment cycle. A typical cycle would require at least 4 ultrasound scans. When the leading follicle reaches the optimum size of (17-22mm), preparations will be made for egg collection. A hormonal test : of oestradiol , progesterone : the hormones that the follciles seccrete , the lh : the hormone that controls the egg relwease : will also be carried out prior to administering hCG, to help determine the timing of egg collection.
The final preparation for egg collection involves a hormonal injection given to the woman 36-40 hours pre-operatively. This mimics the natural process which triggers the eggs to complete their maturation making them ready for fertilisation.


The eggs are collected vaginally using ultrasound guidance, under general or local anaesthesia. The ultrasound probe is introduced into the vagina, the ovaries are visualised and then an aspiration needle (attached to the probe) is passed through the top of the vagina into the follicles. The fluid in each follicle is aspirated and then examined under a microscope for the eggs to be identified. It is difficult to predict the number of eggs available from the ultrasound scan picture. Therefore frequently collection of either more or fewer eggs than antiticipated pre-operatively occurs .
In rare circumstances failure to collect any eggs despite the appearance of follicles on the scan picture occurs . If this occurs, the treatment cycle cannot proceed to embryo transfer and an appointment to see the doctor to discuss future options will be scheduled.
After egg collection, the eggs are incubated for a short time and On the same day the male partner will be asked to collect the sperm sample at the clinic on the day of egg collection. the processessing of the collected sperm is done and then the processed sperm is then added to the eggs and incubated in the laboratory for a further 18-24 hours. Providing that the semen is normal, approximately 65–75% of the eggs will fertilise on average although it can be highly variable from one cycle to another.
The first signs of fertilisation are shown by the presence of two pronuclei within the egg. If this has occurred, the fertilised egg should then divide into two, and subsequently three, four or more cell embryos. The fertilised eggs (now called embryos) are transferred to the uterus 2-5 days after egg collection. A maximum number of embryos that are transferred in to the uterus is decided after discussion with the couple , the dr and the embryologist .transferring more embryos leads to a higher pregnancy rate but more multiple pregnancies and the attendent complications. Usually 2-3 embryos are transferred in out clinic. By 5 days the embryos have developed into blastocysts.

It is important that couple are aware that there is always a possibility that a low proportion or even none of the eggs fertilise. If this occurs the couple will be seen by the clinician to discuss future options.
The embryo transfer procedure is one of the most important events in IVF. It is generally a painless procedure, similar to a cervical smear and on average takes up to 15 minutes. On rare occasions this procedure may take longer. An abdominal scan is generally performed to confirm the correct position of the transfer catheter within the uterine cavity prior to replacement.
After the procedure, women are encouraged to carry on with their normal routine as there is no evidence to suggest that complete bed rest has a positive effect. Additional progesterone in the form of vaginal pessaries or injections are given following egg collection until the pregnancy test is done 2 weeks later. If the pregnancy test is positive the progesterone is continued until the second pregnancy scan at 8-9 weeks.
Cancelled treatment cycles : Unfortunately not all patients respond to the medication and sometimes it may be necessary to abandon the treatment cycle before egg collection. Future management will be discussed and another treatment cycle may be arranged for a later date, perhaps with a different combination of fertility drugs.
The private treatment room in which your mock embryo transfer will take place.
A mock / trial embryo transfer will be carried out before treatment begins. It is normally carried out in the cycle prior to cycle of stimulation.
The mock embryo transfer is a practice for th real embryos are put into the womb. It allows the doctor to take measurements of the womb and to spot any potential problems early, so that we can be prepared when the embryos are put back for real.
The mock embryo transfer will be carried out in a private treatment room. A small plastic tube will be inserted into the womb via the natural opening in the cervix. It is normally painless and takes only a few minutes.

With mild stimulation IVF, the female partner receives a lower dose of fertility drugs over a shorter period of time than with conventional IVF.
A lower dose of fertility drugs is taken for a shorter period of time the fertility drugs taken do not suppress the natural cycle, unlike conventional IVF. This shortens the length of drug treatment by about two weeks and avoids menopausal side effects because lower doses of drugs are used, fewer eggs may be available for collection any embryos of suitable quality that are not used in treatment may be frozen and stored for future use.
